Abstract
Background
General anesthesia (GA) for acute stroke interventions may be associated with inferior functional outcomes. Our goal was to identify physiologic parameters that mediate this association.
Methods
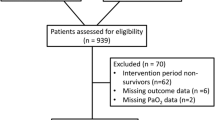
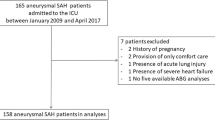
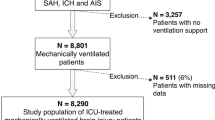
Consecutive patients treated at our institution between August 2007 and December 2010 were identified from a prospective database. Clinical data were then extracted by retrospective chart review. Variables significantly associated with outcome in univariate analysis were also examined in multivariate analysis, controlling for well-established prespecified predictors of functional outcome.
Results
Of the 106 patients identified, 20 were excluded (17 due to the absence of 90-day mRS and 3 due to insufficient anesthetic records). Blood pressure (BP) decreased significantly after induction of GA, but there was no association between BP and outcome. End tidal carbon dioxide values (ETCO2) at 60 and 90 min, however, were significantly associated with outcomes in both univariate and multivariate analyses. Mean ETCO2 in patients with favorable outcomes (modified Rankin Scale (mRS) 0–3) was higher than in those with unfavorable outcomes (mRS 4–6): 35.2 mmHg versus 32.2 (p = 0.03) at 60 min and 34.9 versus 31.9 (p = 0.04) at 90 min. The adjusted odds ratios for poor outcomes for each 1 mmHg decrease in ETCO2 were the same: 0.76 (95 % CI 0.65–0.92; p = 0.004) at 60 min and 0.76 (95 % CI 0.61–0.93; p = 0.01) at 90 min.
Conclusions
While BP decreased significantly in patients undergoing GA for acute stroke intervention, it did not correlate with patient outcome. Decreases in ETCO2 at 30 and 60 min, however, were associated with 90-day mRS.

Similar content being viewed by others
References
Abou-Chebl A, Lin R, Hussain MS, et al. Conscious sedation versus general anesthesia during endovascular therapy for acute anterior circulation stroke: preliminary results from a retrospective, multicenter study. Stroke. 2010;41:1175–9.
Jumaa MA, Zhang F, Ruiz-Ares G, et al. Comparison of safety and clinical and radiographic outcomes in endovascular acute stroke therapy for proximal middle cerebral artery occlusion with intubation and general anesthesia versus the nonintubated state. Stroke. 2010;41:1180–4.
Nichols C, Carrozzella J, Yeatts S, Tomsick T, Broderick J, Khatri P. Is periprocedural sedation during acute stroke therapy associated with poorer functional outcomes? J Neurointerv Surg. 2010;2:67–70.
Davis MJ, Menon BK, Baghirzada LB, et al. Anesthetic management and outcome in patients during endovascular therapy for acute stroke. Anesthesiology. 2012;116:396–405.
Leonardi-Bee J, Bath PM, Phillips SJ, Sandercock PA. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke. 2002;33:1315–20.
Ahmed N, Wahlgren N, Brainin M, et al. Relationship of blood pressure, antihypertensive therapy, and outcome in ischemic stroke treated with intravenous thrombolysis: retrospective analysis from Safe Implementation of Thrombolysis in Stroke-International Stroke Thrombolysis Register (SITS-ISTR). Stroke. 2009;40:2442–9.
Castillo J, Leira R, Garcia MM, Serena J, Blanco M, Davalos A. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke. 2004;35:520–6.
Sandset EC, Bath PM, Boysen G, et al. The angiotensin-receptor blocker candesartan for treatment of acute stroke (SCAST): a randomised, placebo-controlled, double-blind trial. Lancet. 2011;377:741–50.
Kitano H, Kirsch JR, Hurn PD, Murphy SJ. Inhalational anesthetics as neuroprotectants or chemical preconditioning agents in ischemic brain. J Cereb Blood Flow Metab. 2007;27:1108–28.
Curley G, Kavanagh BP, Laffey JG. Hypocapnia and the injured brain: more harm than benefit. Crit Care Med. 2010;38:1348–59.
Higashida RT, Furlan AJ, Roberts H, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34:e109–37.
Nogueira RG, Liebeskind DS, Sung G, Duckwiler G, Smith WS. Predictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI Trials. Stroke. 2009;40:3777–83.
Flint AC, Cullen SP, Faigeles BS, Rao VA. Predicting long-term outcome after endovascular stroke treatment: the totaled health risks in vascular events score. AJNR Am J Neuroradiol. 2010;31:1192–6.
Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38:967–73.
Ito H, Ibaraki M, Kanno I, Fukuda H, Miura S. Changes in the arterial fraction of human cerebral blood volume during hypercapnia and hypocapnia measured by positron emission tomography. J Cereb Blood Flow Metab. 2005;25:852–7.
Muizelaar JP, Marmarou A, Ward JD, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75:731–9.
Rout MW, Lane DJ, Wollner L. Prognosis in acute cerebrovascular accidents in relation to respiratory pattern and blood gas tensions. Br Med J. 1971;3:7–9.
Plum F. Hyperpnea, hyperventilation, and brain dysfunction. Ann Intern Med. 1972;76:328.
Grune F, Kazmaier S, Sonntag H, et al. Moderate hyperventilation during intravenous anesthesia increases net cerebral lactate efflux. Anesthesiology, V XX. 2013;10:1–8.
Sato K, Sadomoto T, Hirasawa A, et al. Differential blood flow responses to CO2 in human internal and external carotid and vertebral arteries. J Physiol. 2012;590:3277–90.
Funding
None.
Conflict of interest
Courtney Takahashi, Ansgar Brambrink, Michael Aziz, Elizabeth Macri, Joshua Raines, Anmol Multani-Kohol, Holly Hinson, Helmi Lutsep, Wayne Clark, and Jeremy Fields declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takahashi, C.E., Brambrink, A.M., Aziz, M.F. et al. Association of Intraprocedural Blood Pressure and End Tidal Carbon Dioxide with Outcome After Acute Stroke Intervention. Neurocrit Care 20, 202–208 (2014). https://doi.org/10.1007/s12028-013-9921-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9921-3