Abstract
Introduction
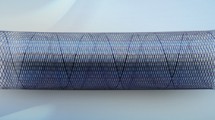
In this study, we analyzed angiographic and histologic aneurysm occlusion of a newly designed flow-diverting device. Visibility and flexibility, as well as occlusions of side branches and neointimal proliferation were also evaluated.
Methods
Aneurysms were induced in 18 New Zealand white rabbits and treated with a braided, “closed-loop-designed” device of nitinol. Additional devices were implanted in the abdominal aorta to cover the origin of branch arteries. Angiographic follow-ups were performed immediately after placement of the device, after 3 months (n = 9) and 6 months (n = 9). The status of aneurysm occlusion (using a five-point scale) and the patency of branch arteries were assessed.
Results
Aneurysm occlusion rates were noted as grade 0 in 2 (11 %), grade I in 1 (6 %), grade II in 1 (6 %), grade III in 9 (50 %), and grade IV in 5 (28 %) of 18 aneurysms, respectively, indicating a complete or near-complete occlusion of 78 % under double antiplatelet therapy. Aneurysm occlusion was significantly higher at 6 months follow-up (P = 0.025). Radiopaque markers provided excellent visibility. Limited device flexibility led to incomplete aneurysm neck coverage and grade 0 occlusion rates in two cases. Distal device occlusions were found in three cases, most likely due to an extremely undersized vessel diameter in the subclavian artery. No case of branch artery occlusion was seen. Intimal proliferation and diameter stenosis were moderate.
Conclusion
The tested flow diverter achieved near-complete and complete aneurysm occlusion under double antiplatelet therapy of elastase-induced aneurysms in 78 %, while preserving branch arteries.







Similar content being viewed by others
Abbreviations
- FD:
-
Flow diverter
- DSA:
-
Digital subtraction angiography
- AA:
-
Abdominal aorta
- SA:
-
Subclavian artery
- ICA:
-
Internal carotid artery
- PED:
-
Pipeline embolization device
- SFD:
-
SILK flow diverter
References
Molyneux AJ, Kerr RSC, Yu L-M et al (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366:809–817
McDougall CG, Spetzler RF, Zabramski JM et al (2012) The Barrow Ruptured Aneurysm Trial. J Neurosurg 116:135–144
Grunwald IQ, Papanagiotou P, Struffert T et al (2007) Recanalization after endovascular treatment of intracerebral aneurysms. Neuroradiology 49:41–47
Gallas S, Januel AC, Pasco A et al (2009) Long-term follow-up of 1036 cerebral aneurysms treated by bare coils: a multicentric cohort treated between 1998 and 2003. AJNR Am J Neuroradiol 30:1986–1992
Kallmes DF, Ding YH, Dai D et al (2007) A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke 38:2346–2352
Fiorella D, Woo HH, Albuquerque FC, Nelson PK (2008) Definitive reconstruction of circumferential, fusiform intracranial aneurysms with the pipeline embolization device. Neurosurgery 62:1115–1120
Lylyk P, Miranda C, Ceratto R et al (2009) Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery 64:632–642
Kallmes DF, Ding YH, Dai D et al (2009) A second-generation, endoluminal, flow-disrupting device for treatment of saccular aneurysms. AJNR Am J Neuroradiol 30:1153–1158
Sadasivan C, Cesar L, Seong J et al (2009) An original flow diversion device for the treatment of intracranial aneurysms: evaluation in the rabbit elastase-induced model. Stroke 40:952–958
Kulcsar Z, Houdart E, Bonafé A et al (2011) Intra-aneurysmal thrombosis as a possible cause of delayed aneurysm rupture after flow-diversion treatment. AJNR Am J Neuroradiol 32:20–25
Turowski B, Macht S, Kulcsár Z et al (2011) Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent): do we need to rethink our concepts? Neuroradiology 53:37–41
Cebral JR, Mut F, Raschi M et al (2011) Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol 32:27–33
Berge J, Biondi A, Machi P et al (2012) Flow-diverter silk stent for the treatment of intracranial aneurysms: 1-year follow-up in a multicenter study. Am J Neuroradiol 33:1150–1155
Fischer S, Vajda Z, Aguilar Perez M et al (2012) Pipeline embolization device (PED) for neurovascular reconstruction: initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology 54:369–382
Maimon S, Gonen L, Nossek E et al (2012) Treatment of intracranial aneurysms with the SILK flow diverter: 2 years' experience with 28 patients at a single center. Acta Neurochir 154:979–987
Becske T, Kallmes DF, Saatci I et al (2013) Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology 267:858–868
Cloft HJ, Altes TA, Marx WF et al (1999) Endovascular creation of an in vivo bifurcation aneurysm model in rabbits. Radiology 213:223–228
Aurboonyawat T, Blanc R, Schmidt P et al (2011) An in vitro study of silk stent morphology. Neuroradiology 53:659–667
Gross BA, Frerichs KU (2013) Stent usage in the treatment of intracranial aneurysms: past, present and future. J Neurol Neurosurg Psychiatry 84:244–253
Cremers B, Kelsch B, Clever YP et al (2012) Inhibition of neointimal proliferation after bare metal stent implantation with low-pressure drug delivery using a paclitaxel-coated balloon in porcine coronary arteries. Clin Res Cardiol 101:385–391
Kamran M, Yarnold J, Grunwald IQ, Byrne JV (2011) Assessment of angiographic outcomes after flow diversion treatment of intracranial aneurysms: a new grading schema. Neuroradiology 53:501–508
Seong J, Wakhloo AK, Lieber BB (2007) In vitro evaluation of flow divertors in an elastase-induced saccular aneurysm model in rabbit. J Biomech Eng 129:863–872
Kulcsár Z, Ernemann U, Wetzel SG et al (2010) High-profile flow diverter (Silk) implantation in the basilar artery. Stroke 41:1690–1696
van Rooij WJ, Sluzewski M (2010) Perforator infarction after placement of a pipeline flow-diverting stent for an unruptured A1 aneurysm. AJNR Am J Neuroradiol 31:E43–44
Dai D, Ding YH, Kadirvel R et al (2012) Patency of branches after coverage with multiple telescoping flow-diverter devices: an in vivo study in rabbits. AJNR Am J Neuroradiol 33:171–174
Asakura M, Ueda Y, Nanto S et al (1998) Remodeling of in-stent neointima, which became thinner and transparent over 3 years: serial angiographic and angioscopic follow-up. Circulation 97:2003–2006
Dai D, Ding YH, Kadirvel R et al (2007) Bone formation in elastase-induced rabbit aneurysms embolized with platinum coils: report of 2 cases. AJNR Am J Neuroradiol 28:1176–1178
Acknowledgments
We would like to thank Admedes Schuessler GmbH, Pforzheim, Germany, for providing the prototype FDs and delivery systems. We would also like to thank the Head of the Department of Experimental Surgery, Prof. Menger, and his team, for supporting this study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simgen, A., Ley, D., Roth, C. et al. Evaluation of a newly designed flow diverter for the treatment of intracranial aneurysms in an elastase-induced aneurysm model, in New Zealand white rabbits. Neuroradiology 56, 129–137 (2014). https://doi.org/10.1007/s00234-013-1296-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-013-1296-9