Abstract
Previous MR studies have established that bilateral transverse sinus stenosis (BTSS) predicts idiopathic intracranial hypertension without papilledema (IIHWOP) in migraine. However, it is uncertain whether BTSS identifies IIHWOP in patients with chronic tension-type headache (CTTH): using cerebral MR venography this study aimed to address this question.
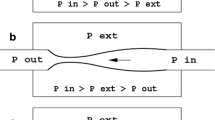
In a prospective study from February 2002 to December 2006, 198 consecutive patients with CTTH underwent MR venography. Of these patients, 58 underwent lumbar puncture to measure cerebrospinal fluid (CSF) pressure. MR venography and lumbar puncture were also performed in 45 agematched control subjects. BTSS was considered present when the signal flow was poor or lacking (flow gap) in the mid-lateral portion of both transverse sinuses. IIHWOP was diagnosed if the patient met the diagnostic criteria for idiopathic intracranial hypertension and did not have papilledema. Among the 198 patients with CTTH who underwent MR venography, 18 (9%) had BTSS. Thirteen of these 18 patients with BTSS underwent lumbar puncture, and nine (69.2%) had IIHWOP. CSF opening pressure was normal in all 45 patients as well as in all 45 controls with normal MR venography.
These data suggest that BTSS on MR venography is associated with increased intracranial pressure in the absence of papilledema in patients with headache mimicking CTTH.
Similar content being viewed by others
References
Friedman DI, Jacobson DM (2002) Diagnostic criteria for idiopathic intracranial hypertension. Neurology 59:1492–1495
Lipton HL, Michelson PE (1972) Pseudotumor syndrome without papilledema. JAMA 220:1591–1592
Marcelis J, Silberstein SD (1991) Idiopathic intracranial hypertension without papilledema. Arch Neurol 48:392–399
Digre KB (2002) Idiopathic intracranial hypertension headache. Curr Pain Headache Rep 6(3):217–225
Huff AL, Hupp SL, Rothrock JF (1996) Chronic daily headache with migrainous features due to papilledema-negative idiopathic intracranial hypertension. Cephalalgia 16:451–452
Mathew NT, Ravishankar K, Sanin LC (1996) Coexistence of migraine and idiopathic intracranial hypertension without papilledema. Neurology 46:1226–1230
Wang SJ, Silberstein SD, Patterson S, et al. (1998) Idiopathic intracranial hypertension without papilledema. A case-control study in a headache centre. Neurology 51:245–249
Silberstein SD, Corbett JJ (1993) The forgotten lumbar puncture. Cephalalgia 13:212–213
Evans RE, Silberstein SD (2002) Diagnostic testing for chronic daily headache. Headache 42:556–559
Quattrone A, Bono F, Oliveri RL, et al. (2001) Cerebral venous thrombosis and isolated intracranial hypertension without papilledema in CDH. Neurology 57:31–36
Higgins JNP, Gillard JH, Owler BK, et al. (2004) MR venography in idiopathic intracranial hypertension: unappreciated and misunderstood. J Neurol Neurosurg Psychiatry 75:621–625
Farb RI, Vanek I, Scott JN, et al. (2003) Idiopathic intracranial hypertension: the prevalence and morphology of sinovenous stenosis. Neurology 60:1414–1418
Fera F, Bono F, Messina D, et al. (2005) Comparison of different MR venography techniques for detecting transverse sinus stenosis in idiopathic intracranial hypertension. J Neurol 252:1021–1025
Bono F, Lupo MR, Lucisano A, et al. (2002) Obesity does not induce abnormal CSF pressure in subjects with normal MR venography. Neurology 59:1641–1643
Bono F, Lupo MR, Lavano A, et al. (2003) Cerebral MR venography of transverse sinuses in subjects with normal CSF pressure. Neurology 61:1267–1270
Bono F, Messina D, Giliberto C, et al. (2006) Bilateral transverse sinus stenosis predicts IIH without papilledema in patients with migraine. Neurology 67:419–423
Headache Classification Committee of the International Headache Society (1988) Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 8 (Suppl 7):1–96
Headache Classification Committee of the International Headache Society (2004) The International Classification of Headache Disorders. Cephalalgia 24:1–160
Karahalios DG, Rekate HL, Khayata MH, et al. (1996) Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies. Neurology 46:198–202
King JO, Mitchell PJ, Thomson KR, Tress BM (1995) Cerebral venography and manometry in idiopathic intracranial hypertension. Neurology 45:2224–2228
Higgins JN, Owler BK, Cousins C, et al. (2002) Venous sinus stenting for refractory benign intracranial hypertension. Lancet 359:228–230
King JO, Mitchell PJ, Thomson KR, et al. (2002) Manometry combined with cervical puncture in idiopathic intracranial hypertension. Neurology 58:26–30
Bono F, Giliberto C, Mastrandrea C, et al. (2005) Transverse sinus stenoses persist after normalization of the CSF pressure in IIH. Neurology 65:1090–1093
Leach JL, Jones BV, Tomsick TA, et al. (1996) Normal appearance of arachnoid granulations on contrast-enhanced CT and MR of the brain: differentiation from dural sinus disease AJNR Am J Neuroradiol 17:1523–1532
Subramaniam R, Tress B, King J, et al. (2004) Transverse sinus septum: a new aetiology of intracranial hypertension? Australasian Radiology 48(2):114–116
Ireland B, Corbett JJ, Wallace RB (1990) The search for causes of idiopathic intracranial hypertension. Arch Neurol 47:315–320
Giuseffi V, Wall M, Siegel PZ, et al. (1991) Symptoms and disease associations in idiopathic intracranial hypertension: a case control study. Neurology 41:239–244
Radhakrishnan K, Ahlskog JE, Cross SA, et al. (1993) Idiopathic intracranial hypertension. Descriptive epidemiology in Rochester, Minn, 1976–90. Arch Neurol 50:78–80
Scher AI, Stewart WF, Ricci JA, Lipton RB (2003) Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain 106:81–89
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bono, F., Messina, D., Giliberto, C. et al. Bilateral transverse sinus stenosis and idiopathic intracranial hypertension without papilledema in chronic tension-type headache. J Neurol 255, 807–812 (2008). https://doi.org/10.1007/s00415-008-0676-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-008-0676-2