Abstract
Background
The underlying mechanism for symptomatic recovery in patients with cerebral venous and sinus thrombosis (CVST) is not clear, although post-acute recanalization and collateral formation have been proposed as possible mechanisms. To identify the occurrence of recanalization and collateral formation among survivors of CVST and explore its association with symptomatic recovery.
Methods
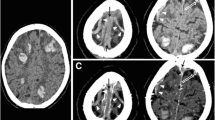
We identified all the patients admitted with CVST over a 5-year period and who underwent initial magnetic resonance (MR) or computed tomographic (CT) venography and a follow-up CT or MR venography between 3 and 12 months after onset. All the images were reviewed by a single observer using the classification for recanalization proposed by Qureshi grade I—partial recanalization of one or more occluded dural sinus with improved flow or visualization of branches; grade II—complete recanalization of one sinus but persistent occlusion of the other sinuses [A—no residual flow, B—non occlusive flow]; grade III—complete recanalization and for collateral formation (grade I—collaterals bypass occluded segment of dural venous sinus but connect within the same sinus; grade II—collaterals bypass occluded segment but connect with a different sinus; grade III—collaterals bypass the occluded segment and connect with different circulation).
Results
A total of 39 patients with CVST (mean age 34.82 [±17.1 SD]; 19 were men) had an initial and follow-up venographic study performed. Of these, 21 patients underwent serial venographic imaging using the same modality allowing a direct comparison. Of the 17 patients who had recanalization during follow-up, 10 patients had grade I recanalization, 7 had grade III recanalization, and 4 had no recanalization. Collateral formation was seen in 8 patients: grade I in 3 patients, grade II in 1 patient, and grade III in 4 patients. The proportion of patients with persistent headaches appeared higher in those with no or partial recanalization than with complete recanalization (5 of 14 patients vs. 0 of 7 patients) and in patients with no collaterals than patients with collaterals (4 out of 13 vs. 1 out of 8). None of the patients experienced any recurrence or new symptoms.
Conclusions
Complete or partial recanalization and collateral formation are seen in a prominent proportion of patients with CVST in the months following initial diagnosis. Further studies need to identify the temporal course and clinical significance of venographic recanalization and collateral formation, and factors influencing venographic changes.





Similar content being viewed by others
References
Bogousslavsky J, Pierre P. Ischemic stroke in patients under age 45. Neurol Clin. 1992;10:113–24.
Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352:1791–8.
Ferro JM, Canhao P, Stam J, Bousser M-G, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004;35:664–70.
Wasay M, Bakshi R, Kojan S, et al. Nonrandomized comparison of local urokinase thrombolysis versus systemic heparin anticoagulation for superior sagittal sinus thrombosis. Stroke. 2001;32:2310–7.
Summers SM. Transverse sinus thrombosis with hemorrhagic venous infarction treated with thrombectomy, endovascular tissue plasminogen activator, and systemic anticoagulation. J Emerg Med. 2009 [Epub ahead of print].
Dentali F, Gianni M, Crowther MA, Ageno W. Natural history of cerebral vein thrombosis: a systematic review. Blood. 2006;108:1129–34.
Stolz E, Trittmacher S, Rahimi A, et al. Influence of recanalization on outcome in dural sinus thrombosis: a prospective study. Stroke. 2004;35:544–7.
English JD, Fields JD, Le S, Singh V. Clinical presentation and long-term outcome of cerebral venous thrombosis. Neurocrit Care. 2009;11:330–7.
Qureshi AI, et al. A classification scheme for assessing recanalization and collateral formation following cerebral venous thrombosis. J Vasc Interv Neurol. 2010;2(3):182–3.
Meijer R, Ihnenfeldt DS, de Groot IJM, et al. Prognostic factors for ambulation and activities of daily living in the subacute phase after stroke. A systematic review of the literature. Clin Rehabil. 2003;17:119–29.
Oujamaa L, Relave I, Froger J, Mottet D, Pelissier J-Y. Rehabilitation of arm function after stroke. Literature review. Ann Phys Rehabil Med. 2009;52:269–93.
Rosser N, Floel A. Pharmacological enhancement of motor recovery in subacute and chronic stroke. NeuroRehabilitation. 2008;23:95–103.
Bonaiuti D, Rebasti L, Sioli P. The constraint induced movement therapy: a systematic review of randomised controlled trials on the adult stroke patients. Eura Medicophys. 2007;43:139–46.
Kidwell CS, Wintermark M. Imaging of intracranial haemorrhage. Lancet Neurol. 2008;7:256–67.
Paciaroni M, Palmerini F, Bogousslavsky J. Clinical presentations of cerebral vein and sinus thrombosis. Front Neurol Neurosci. 2008;23:77–88.
Favrole P, Guichard J-P, Crassard I, Bousser M-G, Chabriat H. Diffusion-weighted imaging of intravascular clots in cerebral venous thrombosis. Stroke. 2004;35:99–103.
Baumgartner RW, Studer A, Arnold M, Georgiadis D. Recanalisation of cerebral venous thrombosis. J Neurol Neurosurg Psychiatry. 2003;74:459–61.
Cakmak S, Derex L, Berruyer M, et al. Cerebral venous thrombosis: clinical outcome and systematic screening of prothrombotic factors. Neurology. 2003;60:1175–8.
Strupp M, Covi M, Seelos K, Dichgans M, Brandt T. Cerebral venous thrombosis: correlation between recanalization and clinical outcome—a long-term follow-up of 40 patients. J Neurol. 2002;249:1123–4.
Genevois O, Paques M, Simonutti M, et al. Microvascular remodeling after occlusion-recanalization of a branch retinal vein in rats. Invest Ophthalmol Vis Sci. 2004;45:594–600.
Einhaupl K, Bousser MG, de Bruijn SF, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis. Eur J Neurol. 2006;13:553–9.
Klauss V, Spannagl M. Thrombin inhibitors and anti-factor Xa agents in the treatment of arterial occlusion. Curr Drug Targets. 2006;7:1285–90.
Jurk K, Schulz AS, Kehrel BE, et al. Novel integrin-dependent platelet malfunction in siblings with leukocyte adhesion deficiency-III (LAD-III) caused by a point mutation in FERMT3. Thromb Haemost. 2010;103(5):1053–64.
Gresele P, Momi S, Berrettini M, et al. Activated human protein C prevents thrombin-induced thromboembolism in mice. Evidence that activated protein c reduces intravascular fibrin accumulation through the inhibition of additional thrombin generation. J Clin Invest. 1998;101:667–76.
Momi S, Nasimi M, Colucci M, Nenci GG, Gresele P. Low molecular weight heparins prevent thrombin-induced thrombo-embolism in mice despite low anti-thrombin activity. Evidence that the inhibition of feed-back activation of thrombin generation confers safety advantages over direct thrombin inhibition. Haematologica. 2001;86:297–302.
Ammollo CT, Semeraro F, Incampo F, Semeraro N, Colucci M. Dabigatran enhances clot susceptibility to fibrinolysis by mechanisms dependent on and independent of thrombin-activatable fibrinolysis inhibitor. J Thromb Haemost. 2010;8:790–8.
Bousser M-G, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol. 2007;6:162–70.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farrag, A., Irfan, M., Guliani, G.K. et al. Occurrence of Post-Acute Recanalization and Collateral Formation in Patients with Cerebral Venous and Sinus Thrombosis. A Serial Venographic Study. Neurocrit Care 13, 373–379 (2010). https://doi.org/10.1007/s12028-010-9394-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9394-6